1. Introduction
Prevention is defined as ‘providing a protective layer of support to stop problems from arising in the first place or from getting worse’; early intervention is defined as ‘providing support at the earliest possible stages when problems occur’.
The Prevention and Early Intervention Network (PEIN) brings together 33 evidence-based practice, advocacy and research organisations seeking to improve outcomes for children, young people and families and to promote quality, evidence-based, informed practice in prevention and early intervention. Over the past decade many of our members have been at the forefront internationally in the design, development, implementation and evaluation of effective prevention and early
intervention programmes and approaches in communities around the country.(1)
This experience leads PEIN to believe that re-orientating child health services towards prevention and early intervention models has a significant contribution to make to achieving better, more equal health outcomes for children and to breaking cycles of poverty and disadvantage.
While valuable interventions can and should be made at any stage across the lifecycle, this paper focuses on the period between the start of pregnancy and three years of age. Research has repeatedly shown that providing high quality prevention and early intervention supports during this critical life stage can create lasting positive outcomes for children and families and prevent difficulties from becoming entrenched in later childhood and adulthood, thus saving money in the longer term.(2)
It is crucial that prevention, promotion and protection are recognised as the most efficient and cost-effective means of promoting health and wellbeing and reducing dependency on acute health and other public services. In particular, PEIN argues for an integrated model of care that organises and manages health and social services so that young children and their parents, from pre-birth onwards, get the information, advice, treatment and care they need when they need it, in ways that
are user-friendly. Thus, these services deliver the desired results and fulfil the child’s right to access preventative care, early intervention, and treatment should they require it.
2. Rationale for Prevention and Early Intervention in Child Health Services
The United Nations Convention on the Rights of the Child (1989).(3) recognises that prevention and intervention strategies during early childhood have the potential to impact positively on young children’s well-being and future prospects. The UN Committee on the Rights of the Child requires States to take all possible measures to improve perinatal care for mothers and babies, reduce infant and child mortality, as well as create conditions that promote the well-being of all young children
during this critical phase of their lives.(4)
Almost 70,000 babies are born in Ireland every year – that is about one baby being born every 7 1⁄2 minutes.
Every pregnant woman and every new born baby will interact with our health services at least 25 times before the baby’s third birthday. This creates a valuable opportunity to provide timely, high quality, evidence-based advice and support to every one of these children and their families. Additionally, when children are in early childhood care and education (ECCE) services there is an opportunity for ECCE Practitioners to observe and support a child’s development, to provide advice to parents and to signpost them to child, parent or family supports and services. ECCE Practitioners and ECCE services also work in collaboration with a wide range of health and social care professionals in identifying children and families with additional needs and in the development and implementation of therapeutic care and family support plans for individual children and their families.
International research as well as a growing body of Irish research(5) clearly indicates that:
- Pregnancy and the early years of life are the most effective times to intervene in the lives of children due to the incredible rate of development of the child during this period
- Early intervention creates positive outcomes for children and families which will endure for their lifetimes
- Early intervention prevents more entrenched health and social difficulties arising later in childhood and throughout adulthood into old age
- Early intervention is cost effective and can save money in the medium to long term(6)(7)
3. Current Irish Policy Context
Child health and wellbeing services in Ireland are being delivered in the context of an evolving policy environment which includes:
- Healthy Ireland 2013-2025 – a framework for Improved Health and Wellbeing)
- Better Outcomes – Brighter Futures 2014-2020 – National Policy Framework for Children and Young People)
- National Maternity Strategy 2016-2026
- Oireachtas Committee on the Future of Healthcare (Sláintecare) Report – May 2017.
The Department of Children and Youth Affairs is currently finalising the National Early Years Strategy which is due for publication in 2018.
Work is currently underway in the Health Service Executive to strengthen and standardise its approach to supporting infant health and wellbeing and to develop the quality of services using an evidence-based approach. This work is taking place under the auspices of the new National Healthy Childhood Programme(8) which will ultimately address the needs of all children from pregnancy to adulthood. The Nurture Programme: Infant Health and Wellbeing(9) is supporting the HSE to develop
quality services in pregnancy and early childhood. Services delivered under the National Healthy Childhood Programme(10) include:
- Health promotion and improvement for parents and children throughout pregnancy and early childhood
- Antenatal supports and maternity services
- Child nutrition and breastfeeding supports
- Child health screening and surveillance services
- Child immunisation services
- Child developmental assessments
In 2017, the HSE established the National Woman and Infants Health Programme11 which is charged with the implementation of the National Maternity Strategy.
Significant regional variations in the accessibility of services, together with often lengthy waiting lists, are denying children timely access to critical health assessments and interventions. These delays can have a serious negative effect on children’s development and lead to a reliance on later and more expensive interventions which are typically less effective than early intervention.
Speech and language difficulties can be of particular concern in disadvantaged areas, where up to half of all children may require a speech and language assessment. Recognising this several Area Based Childhood12 (ABC) programme areas have been working to provide Speech and Language Therapy (SLT) supports in disadvantaged communities over the past number of years. In addition to providing therapeutic supports directly to children, these services provide training and mentoring to
early years practitioners, teachers, and parents and adopt a community based, prevention and early intervention approach that aims to promote and support oral language development, prevent speech and language developmental delays and identify delays early with the aim of making appropriate referrals to HSE SLT services.
The Government has committed to develop a new model of In-School Speech and Language Therapy and to bring the number HSE Speech and Language Therapists up to 1,102 (a 25% increase). The approach used by ABC areas, and the learning from them, should inform the new in-school SLT initiative, which should be extended into early childhood care and education settings as well as schools.(13)
4. Sláintecare Report May 2017
Oireachtas Committee on the Future of Healthcare was established in June 2016 and published its report, The Sláintecare Report14 in May 2017.
The Committee was set up to devise a ten-year strategy for the development of healthcare in Ireland based on consensus between the political parties and groupings.
Key aspects of the Committee’s Terms of Reference included:
- Developing a model based on population health needs
- Reorientating the model of care towards primary and community care where the majority of people’s health needs can be met locally
- Advocating the principles of prevention and early intervention, self-management and primary care services as well as integrated care;
Sláintecare Report – Key Recommendations
- Increase investment in health and wellbeing services by €233m over 10 years;
- Enhance child health and wellbeing budget by €41m over 5 years;
- Re-orientate the model of care towards primary and community care where the majority of people’s health needs can be met locally;
- Free up Public Health Nurses who have training in child health services to carry out child health work as part of the current Nurture Programme -Infant Health and Wellbeing and the HSE’s National Healthy Childhood Programme by hiring 900 more general nurses over 5 years to work in the community with older people and people leaving the acute sector;
- Ensure that parents are supported to meet the emotional development needs of their children as well as their physical health needs through supporting the development of the parent-child relationship during pregnancy and in the early years of the child’s life.
5. Child Health Services Principles
PEIN advocates that our child health services should be underpinned by the following principles:
a) A National Early Years Strategy which recognises every child’s right to preventative healthcare and commits to adopting a prevention and early intervention approach integrated across all children and family services.
b) An integrated “whole of government” approach to child health and wellbeing in recognition that children’s wellbeing is everyone’s business and that it is in everyone’s interest to protect and promote it.
c) Maximise existing skills and resources by improving communication, cooperation and integration across state services and with publicly funded services delivered by the community, voluntary and private sectors.
d) Providing community-based, early intervention and preventative healthcare services within a primary care structure so that children and families can access effective services close to home and when they need them.
e) Providing a multi-disciplinary / cross agency strategy that can deliver an integrated, child- centred response to children and families that present with multiple health and wellbeing needs, in a more effective, timely, consistent and coordinated manner.
f) Operate on the principle of “progressive universalism” – providing universal supports and services to all children and families which are tailored to meet their varying degrees of need, together with additional supports for those children, families and populations with additional needs.
g) Recognise the economic as well as the health benefits of adopting a prevention and early intervention approach and allocate resources accordingly.
h) Achieve a balance between national standardisation and local flexibility so as to meet the particular needs of all communities.
i) Facilitate parents in having their voices heard in a meaningful manner as key partners in supporting their children’s health and wellbeing as well as in the design, delivery and review of services.
j) Provide and promote accessible information on services for expectant mothers, children and their families.
k) Develop a workforce which is of sufficient size to provide for the needs of all children on a timely basis and which has the necessary supports and competencies to provide consistent, evidence-based, quality, child-sensitive, culturally-appropriate services to children and their families.
l) Incorporate accountability mechanisms to ensure that quality assurance standards are maintained.
6. PEIN recommendations for Child Health in Ireland:
1. Commence the implementation of the Sláintecare Report immediately with particular priority given to:
- Re-orientating the model of care towards primary and community care
- Taking a health and wellbeing approach
- Delivering a phased investment to child health and wellbeing services over 5 years
- Creating Child and Family Community Nurses
- Supporting parents in meeting the emotional as well as the physical development needs of their child during pregnancy and early childhood.
2. Establish targets for expenditure across each relevant Government Department which can contribute to improving the health and wellbeing of children. This should be undertaken by the Prevention and Early Intervention Unit in the Department of Public Expenditure and Reform in collaboration with Healthy Ireland.
3. Support women to have a healthy pregnancy and to reduce the risks associated with smoking, drug and alcohol misuse and low birth weight.(15)
4. Provide effective breastfeeding advice prior to birth and enhanced breastfeeding supports at birth and in early childhood.
5. Ensure that parents experience a smooth transition between maternity services and primary care services.
6. Ensure that the achievements of the ABC programme in the health arena are maintained, mainstreamed or replicated as appropriate, providing for continuity of current service delivery.
7. Ensure the early screening of babies and parents for additional support needs and put in place effective referral pathways to services.
8. Ensure that all community based Early Intervention Teams are sufficiently staffed (occupational therapists, child psychologists, physiotherapists, social workers and speech and language therapists) to meet the assessment and therapy needs of children in a timely fashion.
9. Specifically identify Speech and Language support needs early and ensure that needs are met in a partnership between Speech and Language Therapists, Parents, Early Childhood Care and Education Practitioners and Teachers. In particular, extend the proposed In-Schools Speech and Language Programme to early years services, drawing on the lessons of the ABCs, and others with relevant experience.
10. Enhance the preventative and health promotion role of GPs and Practice Nurses as part of the review of the GP contract and the continuation of the phased roll out of Free GP Care for all children.
11. Develop a national Resource Allocation Model to ensure that resources are allocated on the basis of prioritising need, taking into account the need to address the particular service requirements of communities and populations who experience disadvantage.
12. Ensure that a continuum of services is planned and delivered on the basis of local identified need, under the auspices of the Children and Young People’s Services Committees.
13. Deliver services as locally as is practicable and in combined service hubs whenever possible.
14. Ensure that all staff receive core and Continuing Professional Development, delivered locally on an inter-disciplinary and inter-agency basis whenever possible to develop local working relationships.
15. Develop relevant Key Performance Indicators16 and datasets to support staff in the planning and delivery of quality services and ensure that all staff have access to the necessary technology to input, analyse and utilise data to inform their practice.
(1) This includes the Area Based Childhood (ABC) Programme, the Nurture Programme: Infant Health and Wellbeing and the Tusla Development and Mainstreaming Programme, among many others. For further details see www.pein.ie .
(2) Partnership to fight chronic disease (USA), The value of prevention
(3) www.ohchr.org/EN/ProfessionalInterest/Pages/CRC.aspx
(4) UNCRC ‘General Comment No.7: Implementing child rights in early childhood’ (2006) UN Doc CRC/C/G/GC/7/Rev.1
(6) The Impact of Early Childhood on Future Health, Faculty of Public Health Medicine, Royal College of Physicians of Ireland, May 2017
(7) Preparing for Life 2016, Promoting School Readiness and Improving Child Health: Learning from the Evaluation of the Preparing for Life Home Visiting Programme
(8) http://www.hse.ie/eng/about/Who/healthwellbeing/Our-Priority-Programmes/Child-Health-and-Wellbeing/NationalHealthyChildhoodProgramme/
(9) http://www.hse.ie/eng/about/Who/healthwellbeing/Our-Priority-Programmes/Child-Health-and-Wellbeing/NurtureProgramme/
(10) https://www.hse.ie/eng/health/child/nurture/healthy-childhood-prog.pdf
(11) https://www.hse.ie/eng/services/news/media/pressrel/implementation-plan-for-the-national-maternity-strategy-launched.html
(12) https://www.dcya.gov.ie/viewdoc.asp?fn=%2Fdocuments%2F20160729ABCProgrammeOverview.htm
(13) Irish research has found that having a dedicated speech and language service in early years settings enables more children to receive the intervention earlier which would help to remove or reduce a significant disadvantage from them before starting school. See: Hayes, N., Keegan, S. and Goulding, E. (2012) Evaluation of the Speech and Language Therapy Service of Tallaght West Childhood Development Initiative. Dublin: Childhood Development Initiative (CDI).
(14) https://www.oireachtas.ie/parliament/media/committees/futureofhealthcare/Oireachtas-Committee-on-the-Future-of-Healthcare-Slaintecare-Report-300517.pdf
(15) This should occur though health education programmes in primary, secondary and third level education as well as in pre-conception and during pregnancy advice and supports to parents
(16) Building on existing Key Performance Indicators in the HSE
continue reading
Related Posts
Our beloved Hands Up for Children mascot, Peinny, has been hard at work investigating the promises made by political parties […]
The Prevention and Early Intervention Network (PEIN) is thrilled to announce the launch of Hands Up for Children, our campaign […]
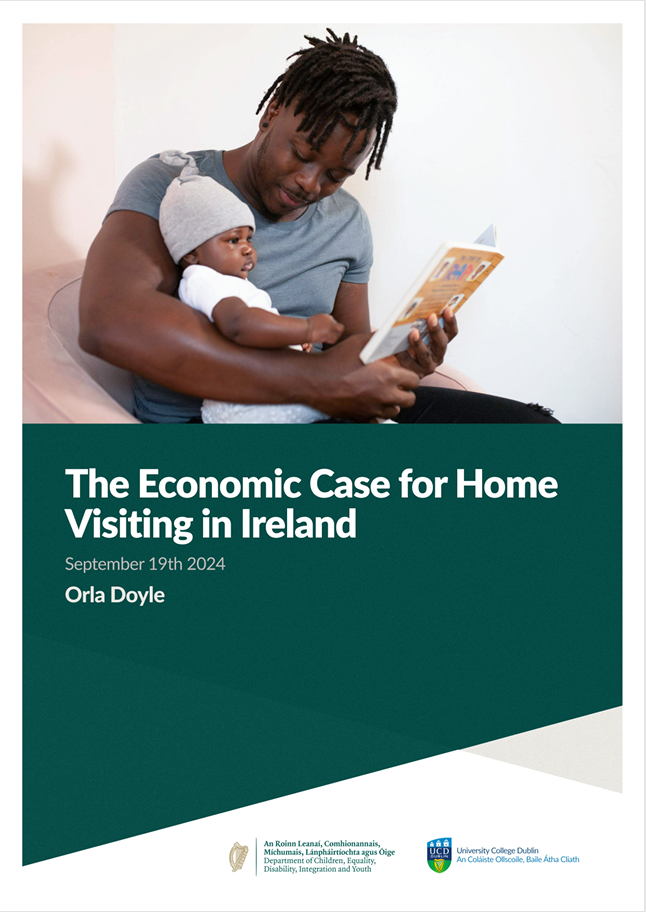
An Economic Study, conducted by Professor Orla Doyle, UCD, which makes the economic case for investing in Home Visiting programmes […]